I entered the world of mental health advocacy kicking and screaming. Some days, quite literally.
Studying English? Easy, I loved literature and writing. Teaching? A way to purvey that love to another generation while parlaying it into a paycheck. Motherhood? An extension of the love my husband and I shared.
Postpartum depression and anxiety? A most unwelcome and unpleasant recalculation in my life’s journey.
For years, I looked for reasons. I hadn’t recalibrated my compass, had I? What had happened to lead to this catastrophic turn of events?
I am not the grand cosmic poomba of all things so I cannot answer those questions with any sort of certainty, but I do know that my struggles awakened a raw, yet steely inner strength I’d never had before. They fostered an empathy of a whole new level for others’ suffering; for the mantle of motherhood and all its ‘come-withs’.
I had to polish some ragged rock I’d gotten caught up on and dragged along on my journey into at least a burnished gem. Something positive had to come out of all that suffering. And perhaps even prevent another woman from travelling the same path.
I started this blog as a way to tell my story, which very few knew. I thought, with complete disclosure, I might open the dialogue for others. At least become an ally in an all too commonly silent struggle. Perhaps I didn’t tackle postpartum directly enough – for many of my discussions and observations were integrated with my life. However, I still haven’t decided if that was/is a failure, for mental health struggles quickly become an intimate part of one’s life, touching all parts of it. It also hinted at some version of depression/anxiety becoming part of my ‘new normal’.
And with my ‘new normal’ so different from my old one, I began to develop further plans for burnishing rocks into gems.
I knew what I wanted to do, but with no clinical experience, I had limitations. I could not mention the word ‘therapeutic’ in any official capacity. I was petrified that if the programs I had in mind reached the end of my personal experience and empathy, that I wouldn’t be able to help someone in crisis.
I embarked on a series of webinars offered by Postpartum Support International. The Social Support Training series, one session every other week, stretched from January to June of last year. While many of the participants were clinicians in the field of maternal mental health, the course was user-friendly and aimed at individuals interested in starting and supporting groups of mothers in various presentations of mental health.
The Social Support Training was the perfect first step toward a solution. It offered a wealth of information – statistical and anecdotal, researched and proven – paired with the assurance that social support people are not meant to be clinicians. They are meant to offer a safe place for mothers to gather and vent, ask questions and talk, discover resources and camaraderie, and just be.
I finished the series a few weeks before I headed to Boston for Postpartum Progress‘ first annual Warrior Mom Conference, the first ever maternal mental health conference for survivors of PMADs. With my new-found knowledge and training, I looked forward to building on that momentum and connecting with other moms doing the same. While I did that, I also found parts of me that hadn’t fully healed. I realized I still had my own work to do and how very complex maternal mental illnesses are.
That fall, my PMAD baby started full-day kindergarten and, though scared as hell, I began formulating plans to kick my ideas into high gear. I applied for a scholarship offered by Postpartum Progress and the National Council for Behavioral Health to be trained in Mental Health First Aid, which I was awarded a few weeks after discovering I was pregnant with my fourth child. I faltered, wondering how I would enact my plans with a newborn baby. But then, they were never my plans anyway. And now I would have the full-circle experience informing my advocacy. Up until now, I’d only ever experienced the postpartum piece of mental health; now I could speak to both pre- and postnatal.
I spent two days in New London, Connecticut with two fabulous humans from Child & Family Agency of Southeastern CT learning how to assess and support a person’s mental health status. Again, the trainers stressed that we were not expected to diagnosis the individuals we come into contact with, but to assess their situation and determine whether they need additional help. We then must help them feel comfortable and safe until such professional help is acquired. The trainers helped me gain even more practical ways to help those in need as a civilian, a concerned individual, an advocate.
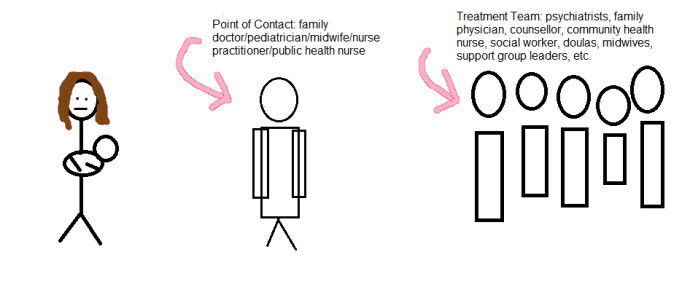
As I sat in that auditorium, surrounded by empathetic professionals and persons, I flashed back to an article I’d read a week and a half earlier. “The Community Maternal Mental Health Professional” on The Burnout Cafe (click image for link) discusses the gap between women who need help and the services available to them. While the central point of contact in this graphic from the article lists a woman’s professional caregivers, and a woman certainly does see these people quite frequently both before and after the baby is born, I would argue another layer of contact needs to be added. If practitioners aren’t well-informed or comfortable dealing with maternal mental health issues, the assessments, diagnoses, and referrals needed will not occur. Having been down that dark hole myself, I am well-versed in those discussions. I can help normalize the feelings a woman may be experiencing, yet not want to admit for fear of retribution to her or her child. I can point her in the direction of practitioners specializing in the exact type of care she so desperately needs.
With my personal experiences and new-found knowledge via recent trainings, I am a point of contact for mothers.
My plans may morph and grow as my own life and family does, but the end goal is the same: