After my third pregnancy, it felt like I saw every specialist under the sun. Midwife, general practitioner, physical therapist, behavioral therapist, chiropractor, podiatrist. It took a lot of work to put me back together physically and mentally.
My schedule hasn’t changed much this time around, except I’m starting my visits prenatally rather than post. And I haven’t hit everyone on the laundry list yet – which is probably a good thing, given I’m already having continuity of care issues.
Today I saw my general practitioner.
It was to be a followup after my visit to a psychiatrist. Shortly before my pregnancy, I’d started with this GP. When discussing my mental health history and current condition, she suggested I get a specific diagnosis from a psychiatrist since what initially presented as postpartum depression was persisting. I’d been continuing care with a LICSW I’d been seeing. Thanks to hospital systems and network nightmares, I’d need to go through 12 CBT sessions at his facility before even seeing the psychiatrist – even though that’s what I’d been doing for years with my own therapist. Already spooked by the red tape and thought of strong psychotropic drugs, I put it all on hold once I found out I was pregnant. I couldn’t start on new meds anyway and didn’t need any additional stress.
Through the guidance of my LICSW and midwife, I decided the benefits of continuing my low dose of meds were greater than the risk of harm during pregnancy. That’s not to say the decision was made lightly. I cut out mostly everything questionable when pregnant. I’d always felt guilt for taking meds in the first place. But after weighing all my options – and a few bad days of trying to wean – the meds stayed.
Now, my GP didn’t know any of this.
When I tried to verify my protocol and discuss my midwife’s suggestion to possibly wean toward the end of pregnancy so the baby would not suffer any possible ill effects of the drug as a newborn, she wondered whether she would’ve advised taking meds at all had she found out earlier in my pregnancy. She said that’s why she wanted the input of the psychiatrist, especially now with a pregnancy, to know exactly with what we were dealing.
Now, this GP is solid. She did not shy away from discussing different prescription therapies. She wanted me to see the psychiatrist to get to the origin point at the bottom of my pit. She is candid, empathetic. Today, however, I felt the doubt and guilt over taking meds during pregnancy try to push up. The doubt that I’m not getting the best possible prenatal care cropped up when she suggested I see an OB in my group rather than only a midwife; her reasoning being that should my situation become critical I would need someone to assess and intervene immediately.
She is following due process. She is looking out for the best interests of me and my baby. She is talented, trained, and professional.
And yet there are gaps in her knowledge of perinatal mood disorders and their treatment.
My midwife, fully aware there is no definitive research saying meds are 100% risk-free during pregnancy, also knows the research that an anxious and/or depressed mother can also have ill-effects on a developing fetus.
My LICSW knows the mental anguish I put myself through in making this decision and that I can’t hang without the meds.
All three are looking out for the best interests of me and my baby. All three are experts in their fields. And yet, at times, all three have told me something different.
Where is the continuity of care in the perinatal period? Yes, the knowledge base is growing. Yes, awareness is spreading. Yes, some practitioners are training themselves to be experts in this ever-growing area. But there isn’t enough widespread know-how. There are gaps in which women can and will fall through.
I haven’t met any of the OBs in the group I visit, but seeing one doesn’t guarantee me swift and effective intervention in the postpartum period. Not taking meds doesn’t guarantee a perfectly formed baby. Taking meds doesn’t even preclude mood disorders.
There is always some mystery involved in making and growing a baby. Insert mood disorders and mental health issues and the lines are blurred even further. Unfortunately, it still falls primarily to the mother to advocate for her own health amidst all the conflicting care.
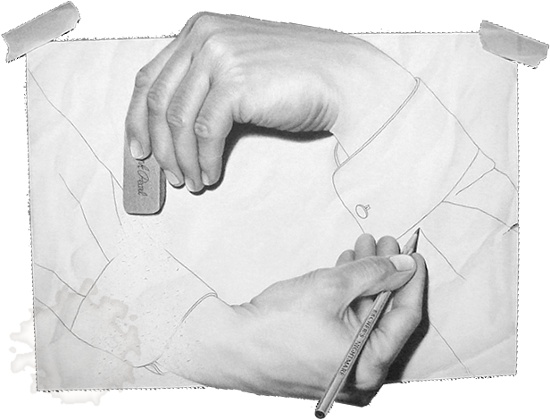
Though still haunted by the postpartum experience in my previous pregnancy, I feel that I can advocate for myself this time. Knowing the danger signs, the markers, the despair, I feel equipped to request and access care as soon as it’s needed. I know who to ask and how to get it. However, that doesn’t mean that all of my helpers will be on the same page. One perinatal hand may very well have no idea what the others are doing – just as I don’t know which specialist I’m seeing unless I know which day it is.
I don’t know your med(s), and I’m not asking, but for several years now the position of the APA has been that being depressed during pregnancy (due to medication withdrawal) is as dangerous or more dangerous to baby than most anti-depressants. Now I get that this is their party line, but they’ve replicated studies and done longitudinal studies, etc. I also have a good friend who had a very bad postpartum period after her last birth. This time around the question wasn’t whether or not to continue medication, it was which medications she would take, full stop. And her baby is perfect.
I would never try to tell you what to do, that’s why you have an army of professionals, and most importantly, yourself. I just want you to know that I support you in your choices. I can only begin to imagine how complicated it must be for you, but I know you and all of your support team will make the best decisions for both you and your baby.
LikeLike
Ruby, you’re always such a blessing. And you know your stuff. I got your lovely response to my last post as well and have not forgotten it. Formulating a response 🙂
LikeLiked by 1 person
No pressure there. I kind of did my crazy, rambling, veering wildly thing that I do sometimes. Okay, that I do often. 😉
LikeLiked by 1 person
Great article and a must read for moms to be and their caregivers in how difficult it is to navigate the system and the care involved in making informed decisions.
LikeLiked by 2 people
And this isn’t my first rodeo! Can you imagine women experiencing this for the first time? Or who haven’t yet realized they even have a problem? There are organizations trying to consolidate care, such as 2020MomProject and Postpartum Support International, there’s still such a long way to go, though.
Thank you for reading and commenting!
LikeLiked by 2 people